Nafees Rahman, who will receive his PhD from the University of Toronto next month, is part of a team from Peter Zandstra’s lab that has developed new technologies that are clearing some of the barriers to having a limitless source of cells to target cancer and other diseases. (Photo: Jovana Drinjakovic)
Bioengineering and professional soccer may not have much in common at first glance, but Nafees Rahman sees a clear link between the career path he chose and his childhood dream.
“Soccer is a team sport and research is also about a team — you can never do it by yourself,” says Rahman, who recently completed his research in the laboratory of Professor Peter Zandstra at the University of Toronto’s Institute of Biomaterials & Biomedical Engineering and will receive his PhD during June convocation.
Rahman specializes in making new blood from scratch as a potential source of cells for life-saving treatments. Together, he and Shreya Shukla, another student from Zandstra’s lab who will receive her PhD next month, have developed new technologies that clear some of the barriers to having a limitless source of cells to target cancer and other diseases. These breakthroughs, described in two recent papers published in Nature Communications and Nature Methods and funded by Medicine by Design and the Ontario Institute for Regenerative Medicine, could lead to new cell therapies for boosting patients’ immune systems against disease, and for cancer immunotherapy, in which immune cells can be engineered to attack tumours.
“A long-term vision in regenerative medicine is to have a renewable source of cells for therapy,” says Zandstra, a University Professor and executive director of Medicine by Design. “Our two papers focused on generating blood and immune cells in the lab that could be used in cancer immunotherapy. Working with our collaborators at U of T, affiliated hospitals and CCRM, we are getting closer to being able to do this.”
Medicine by Design brings together more than 100 researchers from across U of T and its affiliated hospitals, along with hundreds of post-doctoral fellows and graduate students, in collaborative teams to accelerate breakthroughs in regenerative medicine. With its commercialization partner, CCRM, the initiative is also driving Toronto’s regenerative medicine ecosystem and propelling new therapies to market — and ultimately to patients — more quickly.
Researchers around the world are racing to find ways to use stem cells to treat, and even cure, debilitating diseases thanks to their ability to multiply and make all cell types in the body. Naturally occurring stem cells in the bone marrow and cord blood are already being used to bolster the immune systems of patients undergoing cancer treatment that leaves them defenseless against infections. But because the cell grafts come from donors, they are not always available in sufficient supply. Zandstra’s lab, located in the Donnelly Centre for Cellular and Biomolecular Research, is trying to solve this problem by engineering ways to produce these cells in the lab.
Working with Juan Carlos Zúñiga-Pflücker, a professor at U of T’s Department of Immunology and a senior scientist at Sunnybrook Research Institute, the researchers broke down the problem into two areas. First, they found a way to convert pluripotent stem cells — cells that are able to make all the cells in our bodies — into blood progenitor cells, an intermediate state from which all cells in the blood, including immune T cells that fight off infections, are formed. Then they developed new technology for turning blood stem cells into T cells in a way that can be scaled up for clinical use.
“The ultimate goal is to join the two technologies into one pipeline,” says Zandstra. This pipeline would make it easier to develop immunotherapy for cancer using T cells engineered to attack tumours, he adds.
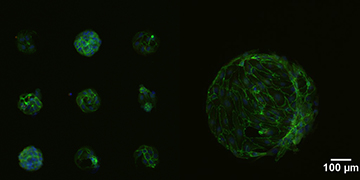
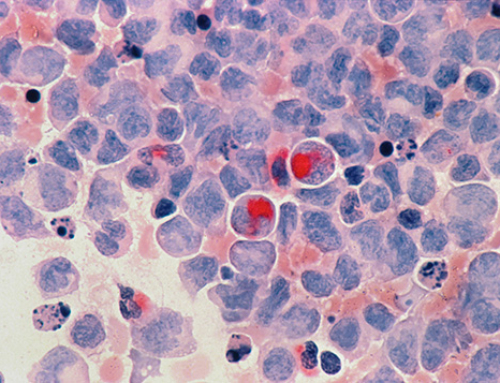
Human stem cell-derived blood progenitor cells in small and large clusters. (Image provided by Nafees Rahman)
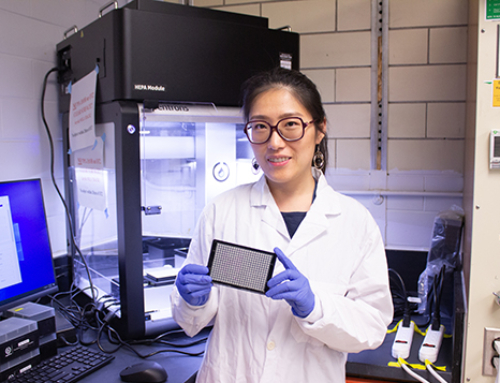
Writing in Nature Communications, Rahman and colleagues describe how simulating the cells’ natural environment during development was key to understanding how blood forms. Instead of spreading the cells evenly across the surface of the dish as usual, Rahman placed them in discrete clusters of different sizes. This allowed him to study how cells talk to each other to influence what kind of blood cells the stem cells turn into. He discovered that larger clusters produced fewer blood cells because the cells secrete a molecule that blocks this process.
“The importance of cell-cell communication during embryonic development is key and it was nice to see this phenomenon replicated in the dish,” says Rahman. “Just by changing cluster size we were able to control how many blood cells we get, resulting in a significant improvement in cell yields.”
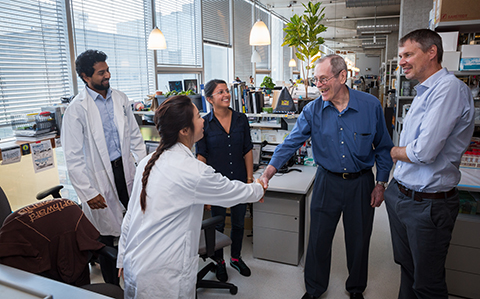
Shreya Shukla (third from right) meets stem cell pioneer James Till (second from right) as he tours the laboratory of Peter Zandstra (right) in July 2015. Also pictured are graduate students Jennifer Ma (front) and Nimalan Thavandiran (left). (Photo: James Poremba)
While blood stem cell grafts can rebuild the patient’s immune system, it takes roughly a year for the immune T cells to appear and start working, leaving the patient vulnerable to life-threatening infections. Shukla’s goal was to protect patients faster.
“Our idea was to use blood stem cells to produce T cells in the lab that we can then transplant into patients,” says Shukla.
But producing immune cells has been hampered by uncertainty over the conditions and ingredients that are required, limiting their potential as medicine.
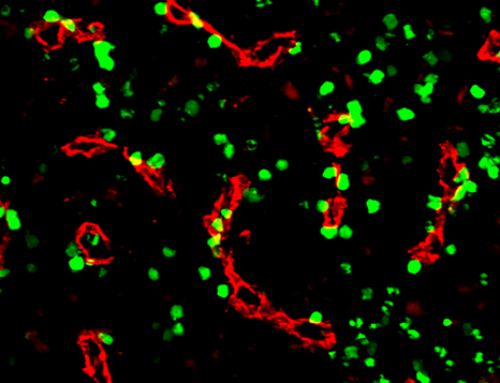
To overcome this challenge, Shukla identified essential components that are needed to spur the blood stem cells to become T cells. As described in the Nature Methods paper, the new technology consists of precisely-defined ingredients and can be scaled up for industrial production.
When injected into mice, the lab-grown T cells can rebuild the immune system in one month, far more quickly than what it takes for the blood stem cells to mature inside the body. If the same is true in humans, it could have immediate applications in cell transplantation.
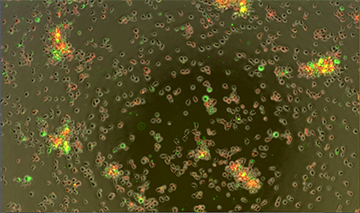
Blood stem cells morphing into immature immune cells, marked in red and green. (Image supplied by Shreya Shukla)
“With our approach, you could move the field to where you have universal, off-the-shelf T cells which could be used in many applications, including cancer immunotherapy,” says Shukla. “You could start with blood or pluripotent stem cells, engineer them to recognize tumours and then turn these into T cells that would rapidly reconstitute the patient’s immune system with cancer-fighting cells.”
“This would get around the problem of the current immunotherapy approach that uses the patients’ own T cells. There can be manufacturing problems with that because there is a lot of variability between different patients’ T cells,” says Shukla.
Shukla is currently testing the technology at a California biotechnology company, where she is doing a six-month internship through the Natural Sciences and Engineering Research Council of Canada’s Create M3 program.
Rahman, too, has swapped an academic lab for a job in biotechnology. Earlier this year, he joined Neurona Therapeutics, a San Francisco startup that aims to generate human stem cell-derived nerve cells for the treatment of epilepsy.
Having played soccer competitively all his life, he is also looking for a team.
“The plan is definitely to play soccer in San Francisco but only for fun,” Rahman says. “My focus now is on learning how to develop stem cell-based therapy going from early discovery in the lab to treating patients.”